Reversing Type 2 Diabetes with Nutritional Ketosis

Virta is a science-based online specialty medical clinic using continuous remote monitoring and intensive coaching to help our patients reverse type 2 diabetes and prediabetes. A unique contributor to our success in this is harnessing and sustaining the metabolic benefits of nutritional ketosis. Admittedly, reversing diabetes is a rather bold goal. By way of contrast, the American Diabetes Association defines type 2 diabetes as a progressive disease whose course at best can be slowed by lifestyle change and medication. Based upon solid science—some old and some new—we beg to differ. Perhaps it’s time for a paradigm change.
There are few times in the lives of medical scientists where we have the opportunity to change the course of a major medical disease; and even fewer cases where we actually succeed in doing so.
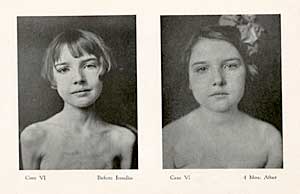
In 1920, Banting’s discovery that injected insulin could control type 1 diabetes (T1D) was such an event. As a result, over the last century, millions of people with T1D have achieved long and productive lives; whereas before 1920 most of them would have succumbed to this insulin-deficiency disease within less than a year.
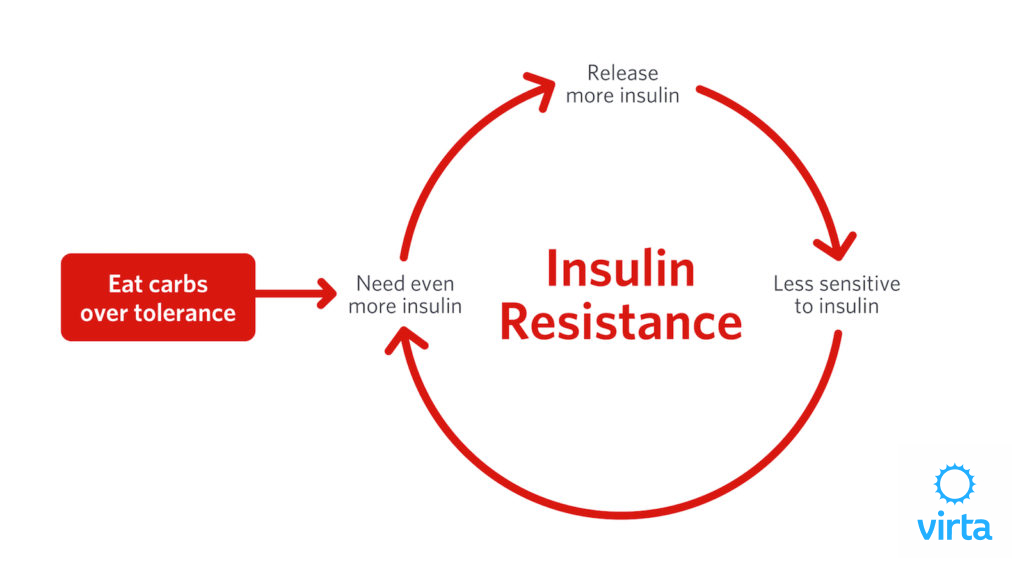
Type 2 diabetes (T2D), on the other hand, is a very different disease that affects hundreds of millions of people. It responds very poorly to injected insulin. Whereas T1D patients cannot make insulin, people with T2D typically make lots of insulin but are resistant to insulin’s effects across a variety of cellular functions. Despite these facts having been known for 5 decades, we are taught that the core components of T2D management are to force the body to make even more insulin or to inject more insulin to overcome the insulin resistance that characterizes this disease. But in study after study, intensive management of type 2 diabetes with medication results in increased side effects and increased body weight, not to mention cost.¹,²

An Opportunity to Change how Type 2 Diabetes Is Not Just Managed, But Actually Reversed
Insulin has many roles as a signaling hormone, but a major one is to get cells to take up blood sugar, most of which usually comes from dietary carbohydrate intake. It helps to think of our muscles and liver as reservoirs for the storage of dietary carbohydrate, which typically comes as a wave of blood glucose following meals. If the streams above these reservoirs are plugged, it can’t get into the reservoir and the "water" (aka, blood glucose) builds up, causing T2D. Seen from this perspective, it makes sense that eating less carbohydrate causes less glucose to accumulate above these reservoirs, and thus less hyperglycemia. At the same time, reducing blood insulin levels facilitates increased fat release from storage, allowing fat oxidation to become the body’s primary energy source.
So in the face of plugged glucose uptake into cells, what is the practical role of restricting dietary carbohydrate? Clearly eating less dietary carbohydrate reduces the need for its uptake into cellular "reservoirs," but are there liabilities of eating less dietary carbohydrates? The quick answer is yes, the first week or two of carbohydrate restriction requires major metabolic adjustments by the body, as well as rapid reductions in diabetes medications. However, after just a few weeks of adaptation to carbohydrate restriction, the benefits of carbohydrate restriction for most people with T2D far outweigh any liabilities. Again, this flies in the face of conventional nutrition teachings, but a bit of history helps understand this dichotomy.
The History of Type 2 Diabetes, Agriculture and Carbohydrates
With the advent of agriculture starting 10,000 years ago, carbohydrate-rich foods have spread around the globe, becoming cultural staples. Wheat, rice, corn, and potatoes have facilitated vast expansions of regional human populations. But this increased reliance on dietary carbohydrates as a primary fuel source seems to have come with a price. In 1987, the renowned geographer and best-selling author Jared Diamond pointed out that archeology tells us that humans lost both height and longevity when they gave up hunting for agriculture.³ And now, just in the last 100 years, we have an epidemic of T2D that seems to have followed our love of sugar and refined carbs as we have shied away from dietary fat.

As recently as just 50 years ago, we had one quarter the prevalence of T2D that we do now. And, for the record, these new cases of T2D are equally as damaging to our bodies as when less than half as many people were afflicted. In other words, this new T2D is just as dangerous as the old T2D, and it can be tightly linked to our increased intake of dietary carbohydrates. But most importantly, we now know precisely how eating more carbs and less fat increases the risk of developing type 2 diabetes. In a few words, it is all about oxidative stress and inflammation. And yes, it is also about ketones, until recently a much underappreciated "alternative fuel" derived from fat.
Oxidative Stress, Inflammation and Type 2 Diabetes
In the last decade, oxidative stress and inflammation have been identified as key underlying causes of T2D.⁴,⁵,⁶ This is potentially transformative, because while T2D has been known to be caused by insulin resistance, despite 50 years of intense research, no one has been able to pinpoint the root cause(s) of insulin resistance. Now we know that ketones at the normal levels characteristic of nutritional ketosis reduce oxidative stress and inflammation, and these benefits can be traced to the actions of genes we are all born with.⁷,⁸ But without modest levels of circulating ketones, these inborn defenses don’t function properly. Stating this another way, eating a high carb diet turns off our defenses against oxidative stress and inflammation, and this deactivation in turn contributes to (if not causes) insulin resistance. Furthermore, as noted above, the more dietary carbs we consume, the greater the tide of glucose needing to be disposed of, which tends to further increase insulin resistance—a classic double whammy.
Can Type 2 Diabetes Be Reversed?
All of this makes for a nice story, but up until recently it has been pretty much a hypothetical game of connecting dots. What’s needed is evidence that T2D in humans can be prevented or reversed by withholding dietary carbs to a level that allows nutritional ketosis to occur. Before insulin was discovered and purified in 1920, going back to the time of the Greeks, the only treatment for diabetes was total starvation or severe carbohydrate restriction, but there was no practical dietary strategy that made this a sustainable solution.
The turning point came in 1976, when Bistrian et al reported seven cases of type 2 diabetes reversal for one year using a very low calorie ketogenic diet.⁹ Following that, there have been multiple attempts to confirm and extend this pioneering report¹⁰,¹¹,¹²,¹³ but all of these clinical studies have used a ketogenic diet for only a few months, followed by a return to diets rich in carbohydrates. Dashti et al¹⁴ reported a series of 30 cases of T2D reversed by a ketogenic diet over 56 weeks, but did not report how many patients were initially enrolled, and they did not report what, if any, medications were taken by these patients.
We have many anecdotes of people with T2D who have utilized a long-term, well-formulated ketogenic diet to lose excess weight, but more importantly many of them also returned their blood glucose values into the normal range for years without medication.¹⁵ While some would claim that this is merely an effect of weight loss per se, Boden et al.¹⁶ demonstrated dramatic improvements in both blood glucose control and insulin sensitivity in just two weeks when a ketogenic diet was eaten to satiety. This is consistent with the observations of Shimazu⁷, Newman⁸, and Youm¹⁷ showing that modest blood levels of ketones directly regulate genes that protect us from oxidative stress, insulin resistance, and inflammation.
And now we at Virta Health are well along with a study in collaboration with Indiana University Health of 262 patients with T2D who are coached to follow a well-formulated ketogenic diet and closely supported by remote continuous care. At 70 days, 92% of these patients remain under our care, HbA1c values were reduced from 7.5% to 6.5%, diabetes medications were reduced by more that 45%, and weight declined by 7%.¹⁸
Which brings us back to the question: can type 2 diabetes be reversed? Given the recent discoveries that beta-hydroxybutyrate triggers dramatic reductions in oxidative stress and inflammation, which in turn reduce the root cause of insulin resistance, there is just one remaining question—can a well-formulated ketogenic diet be followed long term? If the answer to this question is yes, then it follows that type 2 diabetes definitely can be reversed.
Making diabetes biomarkers like HbA1c or fasting glucose better for a few months or even a year is good. Doing it while reducing medication use and reducing excess weight is even better. But if these benefits cannot be sustained, it is just another rollercoaster ride that so many people with type 2 diabetes have previously experienced. The key piece to this puzzle is sustainability.
Getting real people to substantially change what they eat and continue to do so for years is really hard. Most people with T2D have been educated to increase their exercise, avoid dietary fats, eat "healthy carbs," and limit calories. Reversing this failed treatment paradigm takes targeted education and coaching, but this process is aided when it delivers positive and self-reinforcing results. Early and sustained success with improved blood glucose control, reduced medication use, and medically significant weight loss breeds patient empowerment and positive outcomes.
What does the term "diabetes reversal" mean?
- We are calling this “reversal” because most* people can maintain blood glucose values below the diabetes range as long as they maintain a ketogenic diet. However in most* cases, if they return to a carbohydrate-rich diet, their diabetes will return. Thus this is a state of reversal, not a cure.
- We use the term “reversed” if average weekly fasting blood glucose values remain below 126 mg/dl, or if HbA1c remains under 6.5% off all diabetes medications except metformin. We exclude metformin from this medication list because there is no reason to stop it in most people whose diabetes has been reversed. That’s because it has been shown in humans to prevent progression from prediabetes to diabetes, and because it also has been shown in animals to extend life and health.
- While there are many reports of groups of cases with dramatic improvements in diabetes control with short-to-intermediate-term use of ketogenic diets, there are none that report rigorous follow-up of a successful cohort out to a year. Our Virta Health/Indiana University Health Study will be reporting these results at 1 year, 2 years, and then 5 years.
It is our expectation that the majority of our patients will remain in the non-diabetic range after 1 and then 2 years off all diabetes medications other than metformin. If we achieve this goal, we will have laid the foundation to revise the basic treatment paradigm for type 2 diabetes. You can follow our progress and Virta's research on type 2 diabetes reversal and other metabolic disorders by visiting our research page.
* We highlighted the word “most” above because there are no absolutes in medical care. We are often asked if everyone we treat has to stay in nutritional ketosis long term to keep their type 2 diabetes at bay. The correct answer is “no”; some people can maintain their diabetes reversal without appreciable levels of circulating ketones. But they are a minority of the many people we treat, and we are committed to helping each patient chart a personalized course. For the majority, however, particularly those who start with the greatest degree of insulin resistance, nutritional ketosis remains a powerful and necessary tool to reverse this heretofore progressive disease.
The information we provide at virtahealth.com and blog.virtahealth.com is not medical advice, nor is it intended to replace a consultation with a medical professional. Please inform your physician of any changes you make to your diet or lifestyle and discuss these changes with them. If you have questions or concerns about any medical conditions you may have, please contact your physician.
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- The Action to Control Cardiovascular Risk in Diabetes Study Group*. Effects of Intensive Glucose Lowering in Type 2 Diabetes. N Engl J Med 2008; 358:2545-2559. DOI: 10.1056/NEJMoa0802743
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837-53.
- Diamond, J. The Worst Mistake in the History of the Human Race. Discover Magazine, May 1987. <http://discovermagazine.com/1987/may/02-the-worst-mistake-in-the-history-of-the-human-race>
- Duncan BB, Schmidt MI, Pankow JS, Ballantyne CM, Couper D, Vigo A, Hoogeveen R, Folsom AR, Heiss G. The Atherosclerosis Risk in Communities Study. Low-Grade Systemic Inflammation and the Development of Type 2 Diabetes. Diabetes. 2003; 52:1799–1805.
- Donath MY, Shoelson SE. Type 2 diabetes as an inflammatory disease. Nature reviews. Immunology, 2011; 11:98-107.
- Saltiel AR, Olevsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017; 127:1-4.
- Shimazu T, Hirschey MD, Newman J, He W, Shirakawa K, Le Moan N, Grueter CA, Lim H, Saunders LR, Stevens RD, Newgard CB, Farese RV Jr, de Cabo R, Ulrich S, Akassoglou K, Verdin E. Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 2013; 339:211-4.
- Newman JC, Verdin E. β-hydroxybutyrate: much more than a metabolite. Diabetes Research and Clinical Practice. 2014; 106:173-181.
- Bistrian BR, Blackburn GL, Flatt JP, Sizer J, Scrimshaw NS, Sherman M. Nitrogen metabolism and insulin requirements in obese diabetic adults on a protein-sparing modified fast. 1976;25(6):494–504.
- Wing RR, Blair E, Marcus M, Epstein LE, Harvey J. Year-long weight loss treatment for obese patients with type II diabetes: Does including an intermittent very-low-calorie diet improve outcome? Am J Med. 1994; 97:354-362.
- Steven S, Hollingsworth KG, Al-Mrabeh A, Avery A, Aribisala B, Caslake M, Taylor R. Very Low-Calorie Diet and 6 Months of Weight Stability in Type 2 Diabetes: Pathophysiological Changes in Responders and Nonresponders. Diabetes Care 2016; 39:808-815. https://doi.org/10.2337/dc15-1942
- Yancy WS Jr, Foy M, Chalecki AM, Vernon MC, Westman EC. A low-carbohydrate, ketogenic diet to treat type 2 diabetes. Nutrition & Metabolism. 2005; 2:34 https://doi.org/10.1186/1743-7075-2-34
- Wang Y, Snel M, Jonker J, Hammer S, Lamb HJ, de Roos A, Meinders AE, Pijl H, Romijn JA, Smit JWA, Jazet IM, Rensen PCN. Prolonged Caloric Restriction in Obese Patients With Type 2 Diabetes Mellitus Decreases Plasma CETP and Increases Apolipoprotein AI Levels Without Improving the Cholesterol Efflux Properties of HDL. Diabetes Care 2011; 34:2576-2580. https://doi.org/10.2337/dc11-0685
- Dashti HM, Mathew TC, Khadada M, Al-Mousawi M, Talib H, Asfar SK, et al. Beneficial effects of ketogenic diet in obese diabetic subjects. Mol Cell Biochem. 2007; 302:249–56.
- Volek JS, Phinney SD. The Art and Science of Low Carbohydrate Performance. 2012. PP 131-137. Beyond Obesity Publishing, Miami FL.
- Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med. 2005 Mar 15;142(6):403–11.
- Youm Y-H, Nguyen KY, Grant RW, Goldberg EL, Bodogai M, Kim D, et al. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome–mediated inflammatory disease. Nat Med. 2015 Feb 16;21(3):263–9.
- McKenzie A, Hallberg S, Creighton BC, Volk BM, Link T, Abner M, et al. A Novel Intervention Including Individualized Nutritional Recommendations Reduces Hemoglobin A1c Level, Medication Use, and Weight in Type 2 Diabetes. JMIR Diabetes; 2017;2(1):e5.