Reducing the Cost of Insulin by Utilizing Virta's Metabolic Nutrition Therapy

Snap Shot
The increasing cost of health care and medication in the United States is reflective of the burgeoning health crisis associated with chronic diseases like type 2 diabetes (T2D). According to the CDC, 1 in 10 Americans are living with T2D and 1 in 3 has prediabetes. A closer look reveals that the cost of living with diabetes is on the rise, now more than ever. Recent news has pointed to the escalating price of insulin and other diabetes drugs, as well as the extreme measures that some patients have resorted to in order to deal with these rising expenses.
Despite the fact that insulin has been available for almost a century, inexpensive generic versions of this lifesaving drug have limited availability and the price of brand-name versions has increased 3 to 4-fold in the last 15 years. Depending upon the type of diabetes (i.e., type 1 or type 2) and the individual variability in the body’s response to this hormone, daily doses can range from 20 to over 200 units per day. Given that brand-name insulins can go for 20-30 cents per unit, this translates to $5 to $50 per day, or $1800 to $18,000 per year.
When evaluating insulin use, there are three main factors that contribute to the daily dose someone with diabetes needs:
- How much insulin their own pancreas can make
- How responsive (or resistant) they are to this vital hormone
- How much dietary carbohydrate they consume, which then determines how much glucose the body has to dispose of via the action of insulin.
Dietary carbohydrate intake is a major factor driving blood glucose levels, especially in someone who is insulin resistant. If carbohydrate intake is strictly limited, then diabetes medication requirements (including insulin) can drop precipitously. While potentially desirable in the long-term, managing this transition and then sustaining it in a predictable manner can result in dangerous swings in blood glucose unless this process is guided by continuous expert oversight. But, if a patient is able to sustainably reduce or completely eliminate their insulin requirement, the annual cost savings can range from substantial to huge.
Of course, beyond the national and worldwide economic impact of this disease, the burden on patients, both physically and emotionally, can be significant. With around 15-20% of patients with T2D reliant upon insulin therapy, the importance of addressing alternatives to these medications is paramount. But is there a reasonable alternative? How do we replace the role of this essential hormone in the body?
The answer is… we don’t, but we can become less reliant on extra insulin and make better use of that which our body produces.
To accomplish this, we use food as medicine. We have discovered how to safely improve metabolic health such that extra insulin and most other medications to control our blood glucose are no longer necessary. This can occur if we change our food choices to help us control our blood glucose levels and recover our metabolic health.
The Role of Insulin in the Body
Anyone who suffers from diabetes, or who has a loved one affected by the disease, has probably heard of insulin. Unfortunately, insulin use in patients with T2D tends to have a bad reputation, perhaps because it is usually prescribed in patients with advancing disease. Independent of this association with complicated T2D, insulin is nonetheless an important, valuable and essential hormone for life.
Insulin is secreted by the beta cells of the pancreas and acts primarily to maintain normal blood glucose levels. Chronically elevated blood glucose levels, as in type 2 diabetes, can lead to a multitude of health complications, including significant micro and macrovascular damage. Thus, insulin can be regarded as a double-edged sword – too much or too little can be equally dangerous. In this context, the best goal is to get the best glucose control while using the least insulin.
How insulin production is affected is dependent on the type of diabetes. People with type 1 diabetes have lost their ability to make insulin, so they must have a regular exogenous supply. They typically remain insulin sensitive, so their daily dosage tends to stay in the lower range. In contrast to this, people with type 2 diabetes—in the early stages of this disease—retain the ability to make plenty of insulin, but their body becomes increasingly resistant to it. Driven to make more and more insulin, this process eventually overwhelms endogenous production, leading to a need to inject increasing levels of this expensive drug.
When is Insulin Medication Needed for T2D?
When patients can no longer produce the insulin that they need, they must then add exogenous insulin injections to manage their T2D. These patients need the insulin in order to avoid serious health consequences. But why does a patient with T2D who is still capable of making some insulin have to start insulin therapy? We mentioned one of the hallmarks of the development of T2D is insulin resistance. As insulin resistance develops, wherein target tissues like muscles and liver no longer respond to typical levels of insulin, an increasing amount is needed to exert the same effects. Unfortunately, this process often progresses silently for many years before a diagnosis of pre-diabetes or T2D is made. This can mean that a significant amount of damage to the vasculature and to Beta cell function has already occurred by the time of diagnosis. As a result, patients who have been producing high levels of insulin for an extended period of time may have already experienced a decline in Beta cell function to the degree that insulin therapy is required.
Not all patients with T2D need insulin injections at the time of diagnosis, but many will require other glucose lowering medications before insulin becomes necessary. This pharmaceutical-focused standard of care for T2D rarely results in improved metabolic health outcomes, and thus the goal of this treatment is to slow the progression of T2D and its associated complications.
This bleak picture of the usual clinical course of T2D, however, is driven by the previous standard dietary advice to follow a low fat, high carbohydrate diet. But luckily the tide is turning away from this approach. The good news is that many T2D patients – even those who have been diagnosed for years -- are still able to make all the insulin they need. This only becomes possible, however, if they learn to avoid consuming carbohydrates in excess of their individual tolerance. Guiding each individual below their personal carbohydrate threshold is the key to their freedom from expensive and burdensome medications.
To be clear, not all patients with type 2 diabetes are able to be completely withdrawn from insulin and other medications. But if not, as shown in the graph below, in most cases the dosage of these medications can be substantially reduced. It is also important to note that, having reversed one’s diabetes with the Virta Treatment, continued adherence to a moderate-to-high degree of carbohydrate restriction is necessary to sustain these benefits.
Published Results: Virta Treatment Reduces T2D Medication Needs
The Virta Treatment utilizes a well-formulated ketogenic diet delivered in the context of a state-of-the-art remote continuous care app, allowing withdrawal or reduced doses of insulin and other glucose-lowering medications like sulfonylureas. This medication reduction can in turn help to reduce hypoglycemia risks, improve patient safety and cut back on need for emergency medical attention as well as the indirect costs associated with poorly controlled T2D like absenteeism and presenteeism (2).
At 1-year, the Virta-IUH Study was able to demonstrate a significant reduction in medication use, including the reduction or elimination of insulin therapy in 94% of the patients in the continuous care intervention (CCI) (2), as well as the complete elimination of sulfonylurea treatment. And now these reductions in diabetes medications have been shown to continue after two years of the intervention as well (3).
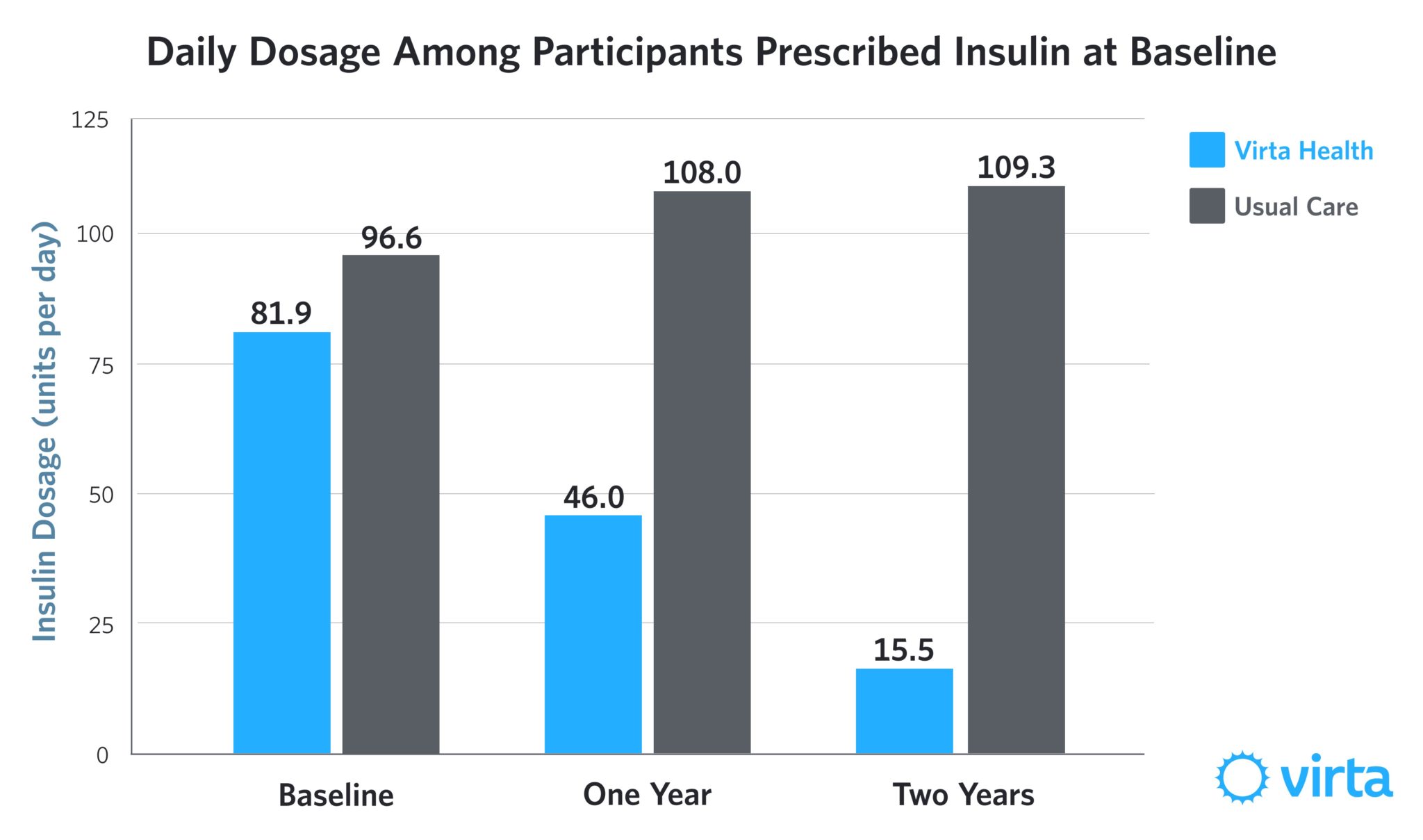
These results indicate that a well-formulated ketogenic diet provided in the context of remote continuous care can demonstrably cut diabetes medication costs by more than half, result in category-leading weight loss* and enable diabetes reversal in about half of the patients after 1 year (2) while sustaining these metabolic health benefits after 2 years (3). And most importantly, the patient-perceived benefits of improved energy, improved well-being, and reduced medication co-pays provides a strong incentive for adherence to this life-changing strategy.
Key characteristics of the Virta Treatment
(1) only dietary carbs and protein are tracked – calories are neither prescribed nor counted
(2) exercise is enabled but not prescribed
(3) the WFKD consists of ‘real foods’ without proprietary formulas or highly refined and chemically-processed meal replacements and snacks.
(4) Because the Virta Treatment promptly, and often dramatically, reduces the need for expensive insulin and other diabetes medications, our daily biometric monitoring and remote continuous care app allows this to be done safely. Virta physicians and coaches track each patient’s status so that the need for these medications can be assessed and adjusted online seven days per week.
Thus, the Virta Treatment — which incorporates a well-formulated ketogenic diet — is the only scientifically proven non-surgical medical strategy that is safe and sustainable over 2 years in the majority of patients who enroll.
Why Virta ‘Works’ and How it is Different
If the Virta Treatment were compared to a ship, the streamlined hull is the Virta virtual technology (aka, the ‘app’) that enables remote continuous contact between the patient and the medical team. Extending this analogy, the medical/coaching and operations teams are the crew, and Virta’s unique scientifically-proven management strategy provides accurate and personalized navigation. And finally, when properly contained within this ‘ship’, the well-formulated ketogenic diet provides a clean-burning and continuous source of power to reverse type 2 diabetes and re-establish metabolic health.
In previous blog posts, we have defined the characteristics of a well-formulated ketogenic diet, its effects on appetite, how its anti-inflammatory effects help reverse T2D, and its effects on sleep and colon health. Many of these benefits are linked to nutritional ketosis, which is admittedly very difficult for many people to maintain in a world awash with sugar and refined carbohydrates. Therefore, it comes as no surprise that most other studies attempting long-term diabetes treatment with short-term low carbohydrate interventions have not had lasting effects on metabolic health.
But given continued biometric monitoring, accurate and personalized guidance, and most of all confidence in the safety and sustainability that many people experience with a well-formulated ketogenic diet, the Virta Treatment is a unique vessel with which to navigate off of expensive diabetes medications and back to metabolic health.
Conclusions
The cost of insulin medication is skyrocketing, and this, combined with the growing number of patients with T2D, paints an alarming picture for future health care costs and patient burden. While insulin is a critical hormone, the amount a patient with T2D needs is largely influenced by dietary carbohydrate intake. A reduction in dietary carbohydrate in combination with the appropriate medical supervision can allow patients to dramatically reduce or eliminate costly insulin and other glucose-lowering medications. A continued effort to move away from the approach of ‘managing’ T2D with multiple medications towards actually improving metabolic health can move us in the direction of reduced health care costs and most importantly, improved patient outcomes.
Visit our research page to learn more about our clinical trial and type 2 diabetes research.
*Based upon published, peer-reviewed outcomes,The Virta Treatment results in both better patient retention and greater weight loss after 2 years than any other non-surgical treatment for patients with T2D
This blog is intended for informational purposes only and is not meant to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition or any advice relating to your health. View full disclaimer
Are you living with type 2 diabetes, prediabetes, or unwanted weight?

- Foos, V., Varol, N., Curtis, BH., et al. Economic impact of severe and non-severe hypoglycemia in patients with Type 1 and Type 2 diabetes in the United States. Journal of Medical Economics. 2015;18(6):420–432
- Hallberg, SJ., McKenzie, AL., Williams, PT., et al. Effectiveness and Safety of a Novel Care Model for the Management of Type 2 Diabetes at 1 Year: An Open-Label, Non-Randomized, Controlled Study. Diabetes Ther. 2018; 9:583–612
- Athinarayanan SJ, Adams RN, Hallberg SJ, et al. Long-Term Effects of a Novel Continuous Remote Care Intervention Including Nutritional Ketosis for the Management of Type 2 Diabetes: A 2-year Non-randomized Clinical Trial. Frontiers in Endocrinology. 2019; 10:348. doi: 10.3389/fendo.2019.00348